A team of researchers headed by BGU's Prof. Iris Shai, has used MRI technology to map body fat. The study, published recently in the Journal of Hepatology, mapped fat deposits in the bodies of hundreds of subjects and measured the effects of a variety of diet regimes on their fat deposits over a long period of time.
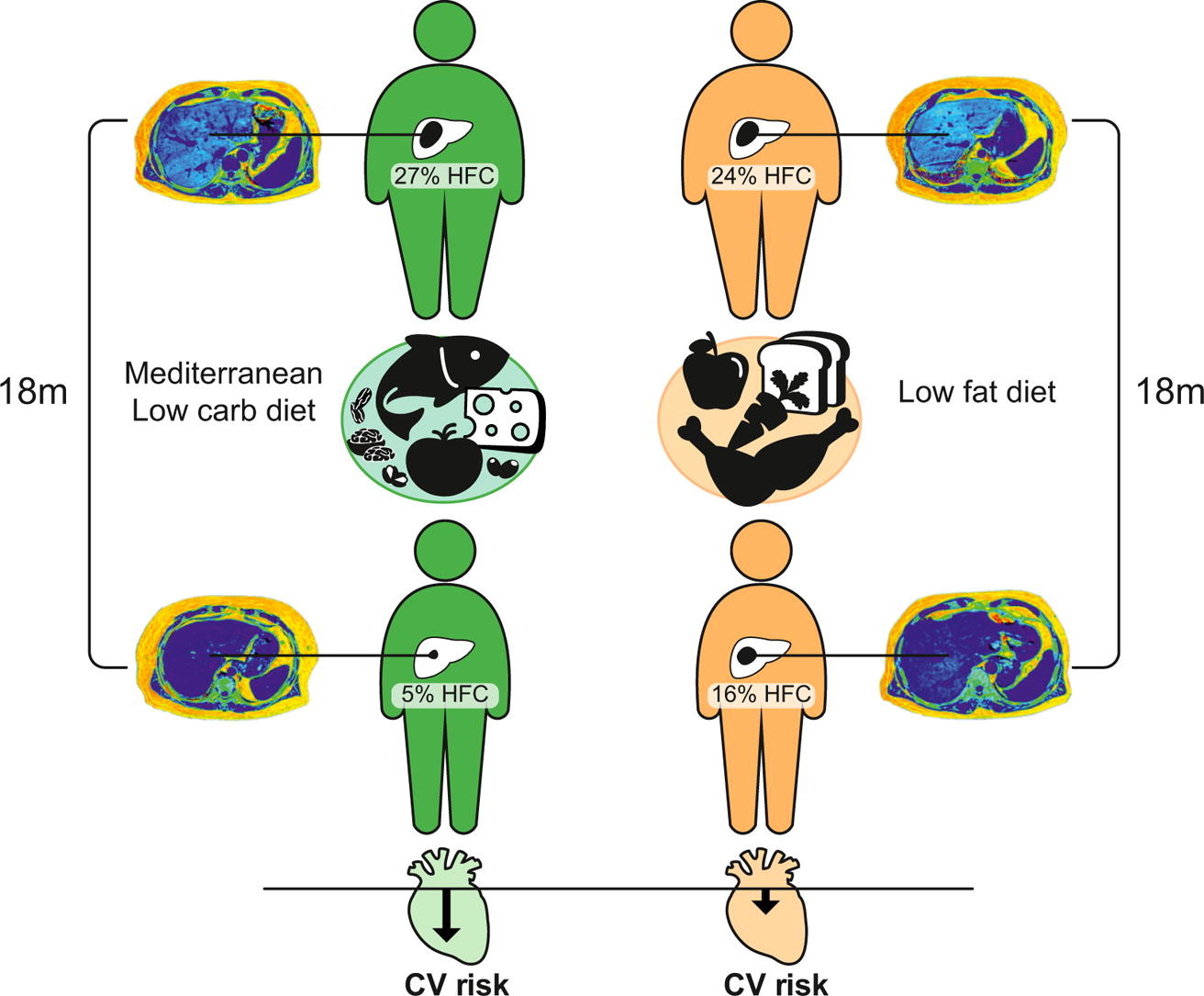
The research team, which included scientists from Leipzig University in Germany and Harvard University, in collaborated with Soroka University Medical Center in Beer-Sheva and the Nuclear Research Center – Negev (NRCN), found that a low-carb Mediterranean diet had a greater effect on reducing fat in the liver, around the heart and in the pancreas, as compared to low-fat diets with similar calorie counts – despite the fact that the level of weight loss was similar. The team also found that moderate physical exercise reduced the amount of visceral fat (stores of fat in the stomach).
The various fat deposits reacted differently to different interactions: Together with moderate weight loss, the amount of liver fat was reduced by 30 percent, fat around the heart decreased by 11 percent (about 70 cc reduction in volume) and visceral fat was reduced by 25 percent. Pancreatic and muscle fat was reduced by only 1-2 percent.
The researchers reported that the dramatic (30%!) reduction in liver fat combined with moderate weight loss is a key element in reducing health risks associated with obesity over the long-term. They also proved that reduction in liver fat is a better predictor of long-term health than reduction of visceral fat, which was previously believed to be the main predictor. The findings are a significant contributor to the emerging understanding that for many obese individuals, excess liver fat is not merely a sign of health risks associated with obesity, including cardiovascular disease and diabetes, but is likely also a cause.
The research team tested the significance of reducing liver fat (in contrast to visceral fat) by comparing the results of some 300 overweight people who followed two reduced-calorie diet regimes: a Mediterranean diet and a low-fat diet. Following the subjects for a period of 18 months demonstrated that changing their respective nutrition habits were consistent with the trial groups that they were randomly assigned to.
In addition, in collaboration with doctoral candidate (now Dr.) Yftach Gepner, a young researcher at Tel Aviv University, Prof. Ilan Shelef and Dr. Dan Schwarzfuchs of Soroka University Medical Center and Prof. Assaf Rudich from BGU, each participant was subjected to a full-body MRI exam in order to analyze the distribution of body fat before, during and after the trial period.
The CENTRAL study is believed to break significant ground towards developing personalized nutritional protocols to address a variety of specific fat deposits using MRI technology, the most precise method currently available for mapping and quantifying fat deposits throughout the human body and for understanding their significance and the role they play.
The CENTRAL study, unprecedented in both its length and breadth, contributes a vast database, consisting of thousands of body images for finding and mapping fat deposits in the human body (it turns out that during a person's lifetime, fat cells move between body parts and that fat plays a variety of health roles, from defense to neutral to poisonous). By following the extent and breadth of these changes over time the researchers, who have developed technologies to quantify specific types of fats, have now paved the way for deeper, more precise understanding of the dynamics of weight loss during a diet period.
As a group, obese people are at higher risk of a variety of diseases than thin people, particularly heart disease, cardiovascular complications and Type 2 diabetes. However, with the growth in obesity rates around the world – some 24 percent of Israeli adults are overweight, and more than 40 percent in the United States – it turns out that the risk that accompanies obesity is more characteristic of certain sub-groups of obese individuals than others. Therefore, one of the most important challenges researchers face today is identifying the sub-groups, or "types" of obesity in the population, and developing treatments with a goal of improving their health in a more unique way.
For example, it turns out that when fat deposits are stored in the abdomen, there is a greater risk of "cardio-metabolic "disease than when the excess fat is stored under the skin. This understanding, alongside other characteristics of visceral fat, suggested that visceral fat is a central cause of obesity-related illness, and that the effectiveness of a variety of treatments should be tested for their specific abilities to reduce visceral fat deposits.
While fat accumulates in the abdomen region, the percentage of fat in the liver also rises for most obese people. The impact of this build up is still a matter of debate (the classic 'chicken-and-the-egg' dilemma: There is still no agreement whether "fatty liver disease" is a disease outright, and many experts believe that without further changes to the liver, like development of infections and/or fibrosis (development of proteins outside cells), there is no significant health risk). Therefore, there are currently no treatments specifically intended to treat fatty liver, other than general advice to lose weight.
Despite similar levels of weight loss, subjects who maintained a Mediterranean diet fared better than those who maintained a low-fat diet according to several indices used to measure risk for heart disease and diabetes. According to three indices used to measure a patient's likelihood to develop heart trouble over the coming 10 years – indices factoring a range of various parameters, including gender and age of the participant, fat and sugar levels in the blood and blood pressure –more significant reductions in the risk of heart disease were found for the participants who followed Mediterranean diets.
The difference between the two groups remained statistically significant even after adjusting for the participants' weight loss, so that the reduction in the risk of heart disease is the result of the impact of a healthy diet even more than the diet's ability to cause weight loss.
The study's most important discovery, however, was reached when researchers tested the dependence of the advantage of a Mediterranean diet over other diet regimes as measured on the reduction of visceral fat or liver fat: While adjusting for the reduction of visceral fat did not erase the statistically significant difference between the diets, adjusting for the (higher) level of reduction in liver fat did erase this gap. This finding supports the possibility that reducing liver fat does not simply reflect, but rather mediates the relationship between dietary choices and reduction of future health risks related to heart disease.
Prof. Shai: "Healthy nutrition, while also maintaining consistent, moderate weight loss, has a much more dramatic impact on levels of body fat related to diabetes, heart disease and cardio-vascular disease than we previously thought. This study could help hone future medical protocols to make them more specifically appropriate for particular types of fat being treated and preferred strategies." Prof. Shelef, Director of Imaging at Soroka University Medical Center added, "This study supports other recent studies that demonstrate the precision of MRI technology in measuring fat quantities in the liver. At the same time the development of similar technologies that could one day present alternatives to taking liver biopsies from patients and will allow repeat measurements in order to adjudicate a particular obese patient's level of health risk, as well as his/her response to treatment."
Currently the group is completing an additional clinical trial – (Direct Plus) that will consider the question of whether a green Mediterranean diet (a proposed improved version of the Mediterranean diet, rich in polyphenols derived from green plants) has an advantage in influencing liver fat and other body systems like the brain, genome, microbiome, heart, and other fat deposits. This clinical trial will join an impressive list of nutrition trials led by Prof. Iris Shai that are unprecedented in their scope, length of study and the use of groundbreaking technology to answer questions about basic nutrition. These trials have already played an important role in undermining conventions and transforming medical protocols around the world.
Media Coverage:
JPost
Israel 21C
The Times of Israel