A new, long-term diet study published in the high impact American Heart Association journal, Circulation, used MRI imaging technology for the first time to plot the diverse changes in an array of body organ fat storage pools during 18 months of Mediterranean-low-carb (Med-LC) and low-fat diets with and without moderate physical exercise.
The CENTRAL MRI is a randomized, controlled trial conducted at Ben-Gurion University of the Negev (BGU), in collaboration with the Dimona Nuclear Research Center and Soroka University Medical Center in Israel, as well as Harvard University and Leipzig University in Germany. The research group, led by Drs. Iris Shai, Yftach Gepner, Ilan Shelef and Dan Schwarzfuchs from BGU and Dr. Meir Stampfer from Harvard University, sought to assess how distinct lifestyle strategies would impact specific body (adipose) fat deposits.
To map these deposits, they collected an unprecedented quantity of whole body MRI data in benchmark six-month and 18-month scans, each with 300 data points, from moderately overweight to obese men and women.
“Weighing patients or using blood tests to detect changes, hasn't, until now, given us accurate pictures, literally, of how different fat deposits are impacted disproportionately by diet and exercise," says Prof. Iris Shai, the primary investigator of the CENTRAL MRI trial, “These findings suggest that moderate exercise combined with a Mediterranean/low carb diet may help reduce the amount of some fat deposits even if you don't lose significant weight as part of the effort."
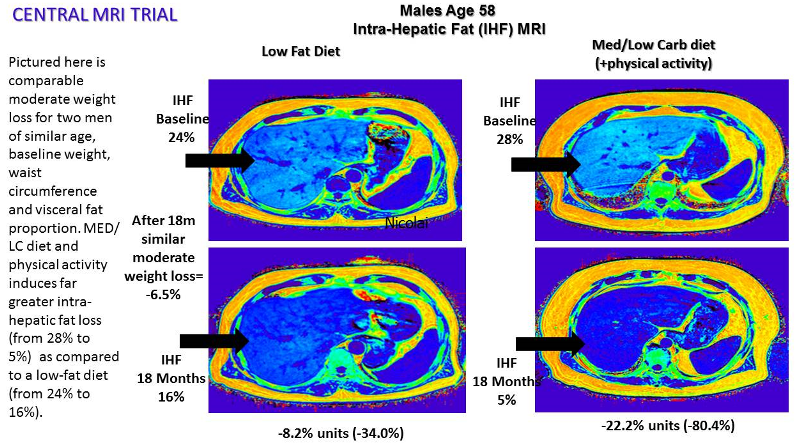
In the study, even with only moderate weight loss, the Med-LC diet was found to be significantly superior to a low-fat diet in decreasing some of the fat storage pools, including visceral (abdominal deep), intra-hepatic (liver), intra-pericardial (heart), and pancreatic fats. However, fat deposits in renal-sinus (kidney), femoral-intermuscular or the cervical (neck) were only altered by weight loss and not by specific lifestyle strategies.
The various fat deposits exhibited highly diverse responsiveness to the interventions, along with moderate, long-term, weight loss. In general, the greatest fat deposit decreases were hepatic (-29 percent), visceral (-22 percent) and intra-pericardial (-11 percent). Pancreatic and femur intermuscular fat deposits were only reduced one to two percent.
"We learned in this trial that moderate, but persistent, weight loss may have dramatic beneficial effects on fat deposits related to diabetes and cardiovascular diseases," Prof. Shai explains. A Mediterranean diet, rich in unsaturated fats and low in carbohydrates, was a more effective strategy than an iso-caloric low-fat diet to dramatically reverse morbid fat storage sites.
The 18-month trial included 278 sedentary adults in an isolated workplace, the Nuclear Research Center, with a monitored lunch provided. The participants were randomized to iso-caloric low-fat or Med-LC diet+28gr of walnuts per day with or without an added moderate workout at least 3 times weekly and a supervised, free gym membership.
The CENTRAL MRI trial followed the groundbreaking DIRECT two-year trial (NEJM 2008) and its four-year follow-up (NEJM 2012). These found that Med-LC diets were effective in improving the cardio-metabolic state and in reversing carotid atherosclerosis (Circulation 2010). Based on those findings, the researchers asked whether internal body fat redistribution, rather than mild weight loss differences between the diets, may underline the significant health benefits attributed to Med-LC diets.
The researchers also found that the decline in hepatic fat and each one of the abdominal fat deposits had specific related health outcomes. After controlling for several parameters, losing visceral fat or hepatic fat were independently associated with improved lipid profile. Losing deep subcutaneous fat was associated with improved insulin sensitivity, and losing superficial subcutaneous fat remained neutral, except for association with decreased leptin hormone.
“In conclusion, the CENTRAL study demonstrates that improving nutritional quality and being physically active can improve cardio-metabolic risk markers through changes in visceral/ectopic fat deposits that are not reflected by changes in body weight alone," Prof. Shai says.
Shai is a member of the The S. Daniel Abraham International Center for Health and Nutrition, and the Department of Public Health, Faculty of Health Sciences at BGU.
The CENTRAL trial was supported by grants from: The Deutsche Forschungsgemeinschaft (DFG): SFB1052; the Deutsche Forschungsgemeinschaft, Obesity Mechanisms, The Israel Science Foundation (ISF), Israel Ministry of Science and Technology (grant # 3-13604), and the Dr. Robert C. and Veronica Atkins Research Foundation.
"Effect of Distinct Lifestyle Interventions on Mobilization of Fat Storage Pools: The CENTRAL MRI Randomized Controlled Trial"
CENTRAL MRI Research Group: Iris Shai, Yftach Gepner, Ilan Shelef, Dan Schwarzfuchs, Assaf Rudich, Meir J. Stampfer, Hila Zelicha, Lilac Tene, Anat Yaskolka Meir, Gal Tsaban, Noa Cohen, Nitzan Bril, Michal Rein, Dana Serfaty, Shira Kenigsbuch, Oded Komy, Arik Wolak, Yoash Chassidim, Rachel Golan, Hilla Avni-Hassid, Avital Bilitzky, Benjamin Sarusi, Eyal Goshen, Elad Shemesh, Yaakov Henkin, Michael Stumvoll, Matthias Blüher, Joachim Thiery, Uta Ceglarek.
Media Coverage:
Israel21C