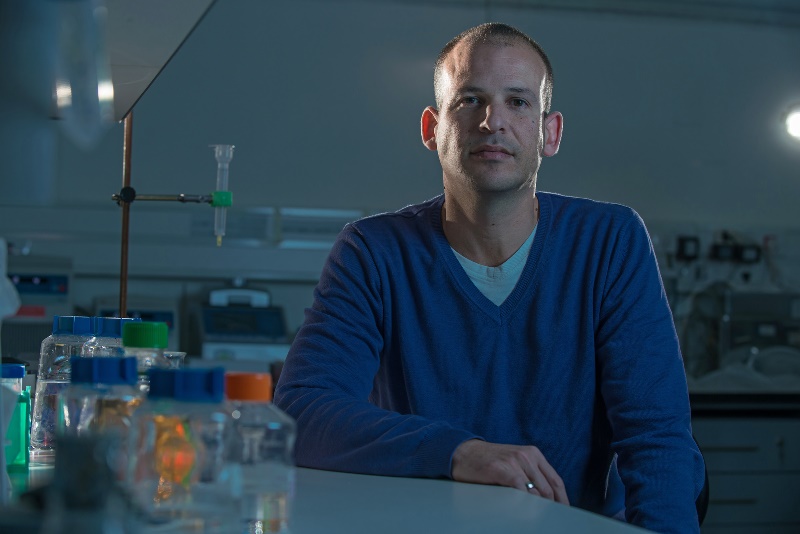
Dr. Niv Papo is developing new proteins that promise to aid in both the diagnosis and treatment of cancer.
A molecular biologist doing protein engineering and cancer imaging, Papo is working to develop new molecules that can recognize cells as being cancerous. This specificity – the ability to differentiate between cancerous and normal cells – stands in sharp contrast to existing cancer therapies, like chemotherapy. Targeting both healthy and malignant cells, chemotherapy often causes hair loss, nausea and weakness, among other side effects.
A member of the Avram and Stella Goldstein-Goren Department of Biotechnology Engineering and the National Institute for Biotechnology in the Negev, Papo has already earned significant recognition for his work. In October 2013 he received the Young Investigator Award from the US-based Prostate Cancer Foundation (PCF) "This is a great honor for a young researcher such as myself. The award will open many new scientific opportunities for my research group on the way to accomplishing our main goal, which is to promote the development of the next generation of prostate cancer therapeutics, including molecular imaging agents and targeted drug delivery agents," he says modestly. This award came shortly after he received a highly prestigious €1,625,000 European Research Council (ERC) Prize for 2013. “This prize enables me to work with the best students and the best equipment. Of course, this helps guarantee success."

The work of Papo and his research team falls under the umbrella of “theranostics," a process of diagnostic therapy involving new medications and hand-tailored treatment for individual patients. A main part of personalized medicine, theranostic processes can, for example, help identify and treat metastases at the same time.
Pointing to the flexibility built into this process, Papo explains, “In diagnostics, we want the imaging agents to do their job and clear out quickly from the system. But with therapy, we want the drugs to stay, and can engineer them to remain in the body longer."
Antibodies, which are currently used in medical imaging, have the disadvantage of being large, and circulating in the body for weeks. Smaller and with shorter half-lives, Papo's engineered protein-based drugs are secreted from the body quickly.
“Our method allows us to design a protein with optimized pharmaceutical properties. This provides greater control of factors such as the protein's distribution in the body and how long it remains. This type of control is beneficial for both therapy and diagnostics," says the researcher.
Papo also believes identifying and developing the “magic bullet" drug will help doctors inhibit cancer and open up a new generation of anti-cancer therapeutics.
At this stage, Papo and members of his research group have already developed the materials and are improving their performance potential. “We are now working to enlarge the ability of a specific drug to affect a wider spectrum of cancers," he says. “The spectrum of cancer types is very broad. You can pick any target and design a drug based on this approach for any cancer. You can choose any compound and make it a good binder for any receptor connected to any cancer cells." So while the scientists are now focusing on prostate cancer, they are confident that the engineered protein compounds can also work on cancers of, say, the breast, brain or lung.
In their work, the researchers create libraries of protein-based drugs. Papo explains that while there are hundreds of millions of different mutations, the compounds' compositions differ very little from each other. The scientists select only those that bind the target through what is called “directed evolution." This imitates natural evolutionary processes, where proteins adapt to new environments, like temperature change. “We are not improving adaptation, but making proteins bind better to relevant targets," he stresses.
Papo and his team are imitating a natural evolutionary process, but of course, they don't have millions of years in which to work. To suit their rather limited time frame, they use yeast cells that reproduce quickly in test tubes and mimic, in weeks, natural processes that take eons. There is further time pressure because of the rapid rate at which cancer cells develop resistance.
Having joined the BGU faculty in 2011 after post-doctoral research at Stanford University, Papo has never looked back. “For young faculty like me, BGU is a great place to be. Researchers and students here are at the highest level. The University nurtures an atmosphere that is both collegial and competitive – in the best sense. There is great cooperation and friendship both in and out of the labs and classrooms."
Papo adds that BGU's proximity to the Soroka University Medical Center offers the great advantage of cooperation with oncologists and imaging specialists. “Most universities and research institutes do not provide these opportunities," he says.
The challenges of building a lab while helping to raise a ten-year-old son and an active pair of six-year-old twins are significant, and leave little time for hobbies. Papo nevertheless manages to windsurf, play tennis and take frequent camping trips with his wife and children.
“I wouldn't be honest if I said that I didn't feel responsibility for the lives of people who might be saved by these medications. I often take this home with me and find myself thinking about everyone and hoping we're all on the right track."